Don’t Let Blood Clots Be the Silent Killer: Spotting the Warning Signs
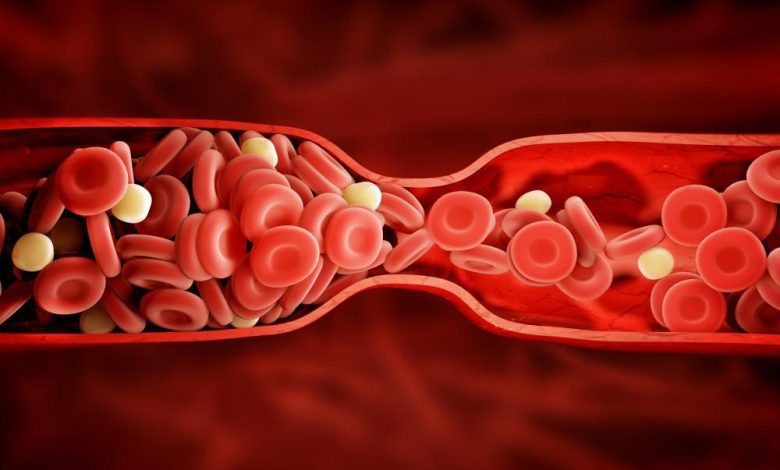
Blood clots can be a silent killer if they go undetected. Clots are the leading cause of pulmonary embolism, a serious medical condition in which a clot blocks a pulmonary artery, causing difficulty breathing and, in extreme cases, death. Knowing the warning signs of blood clots is essential to prevent them from becoming fatal. In this blog post, we’ll discuss what blood clots are, the dangers associated with them, and how to spot the warning signs. Don’t let blood clots be the silent killer – read on to learn more.
What Are Blood Clots and Pulmonary Embolism?
Blood clots are gel-like masses of blood that form in response to injury or to prevent excessive bleeding. They are a necessary part of the body’s natural healing process. However, blood clots can become dangerous when they form unnecessarily or fail to dissolve after healing. This can lead to serious health conditions such as pulmonary embolism.
Pulmonary embolism occurs when a blood clot travels through the bloodstream and becomes lodged in the arteries of the lungs. This blocks blood flow and can cause symptoms such as shortness of breath, chest pain, and coughing up blood. In severe cases, it can even be fatal.
Blood clots and pulmonary embolism can be caused by various factors, including prolonged immobility, surgery, certain medical conditions, and medications. It is important to be aware of the warning signs of blood clots, which can include swelling, redness, warmth, and tenderness in the affected area.
Understanding what blood clots and pulmonary embolism are is crucial for recognizing the symptoms and seeking prompt medical attention. In the next sections, we will explore the causes, warning signs, diagnosis, treatment, and prevention of these life-threatening conditions. Stay tuned to learn more and protect yourself from the silent killer of blood clots.
Causes of Blood Clots and Pulmonary Embolism
Blood clots and pulmonary embolism can be caused by various factors. One of the most common causes is prolonged immobility, such as sitting for long periods during travel or bed rest after surgery. When we are not active, blood can pool in our legs and increase the risk of clotting. Certain medical conditions, such as cancer, heart disease, and autoimmune disorders, can also increase the likelihood of blood clot formation. Tests like geneType risk assessment should be considered to understand the likelihood of developing cancers, blood clotting conditions, and other hereditary diseases.
Medications can also play a role in the development of blood clots. Hormonal contraceptives, including birth control pills and hormone replacement therapy, can increase the risk, especially in women who smoke or have other risk factors. Other medications, such as certain types of chemotherapy drugs, can also contribute to blood clot formation.
Inherited conditions that affect blood clotting, such as Factor V Leiden mutation or antiphospholipid syndrome, can increase the risk of blood clots. Additionally, obesity, smoking, and age can all be contributing factors.
Understanding the causes of blood clots and pulmonary embolism is essential in identifying and managing risk factors. By being aware of these causes, we can take proactive steps to prevent blood clots and keep ourselves safe from this silent killer.
Warning Signs of Blood Clots and Pulmonary Embolism
Blood clots and pulmonary embolism can be life-threatening, but knowing the warning signs can save your life. Paying attention to your body and recognizing the early signs of blood clots is crucial for prompt medical intervention. Common warning signs of blood clots include swelling, redness, warmth, and tenderness in the affected area. For example, if you notice sudden swelling or pain in your leg, it could be a sign of a deep vein thrombosis (DVT), which is a blood clot in the deep veins of the leg.
When it comes to pulmonary embolism, symptoms can be more severe. Shortness of breath, chest pain, rapid breathing, and coughing up blood are some of the key warning signs. These symptoms should never be ignored, as they may indicate that a blood clot has traveled to the arteries of your lungs.
If you experience any of these warning signs, it is important to seek immediate medical attention. Early detection and treatment can prevent serious complications and even save your life. So, listen to your body, be aware of the warning signs, and take action if something feels off. Don’t let blood clots be the silent killer – educate yourself and protect your health.
Diagnosis of Blood Clots and Pulmonary Embolism
Diagnosing blood clots and pulmonary embolism is a crucial step in preventing serious complications and ensuring prompt treatment. If you suspect you may have a blood clot or pulmonary embolism, it is important to seek medical attention immediately.
To diagnose blood clots, your doctor may start by performing a physical examination and reviewing your medical history. They may ask about any recent surgeries, medications, or medical conditions that could increase your risk of blood clots. They may also order diagnostic tests, such as a Doppler ultrasound, to visualize the blood flow in your veins and identify any clots.
For pulmonary embolism, your doctor may order a series of tests to confirm the diagnosis. These tests may include a computed tomography (CT) scan, which uses a series of X-rays to create detailed images of your lungs and blood vessels. They may also perform a ventilation-perfusion scan, which evaluates the flow of air and blood in your lungs.
In some cases, additional tests, such as blood tests or electrocardiogram (ECG), may be performed to assess your overall health and determine the severity of the condition.
It is important to remember that diagnosing blood clots and pulmonary embolism requires medical expertise and specialized tests. If you experience any warning signs, don’t hesitate to seek immediate medical attention to ensure an accurate diagnosis and appropriate treatment.
Treatment for Blood Clots and Pulmonary Embolism
When it comes to treating blood clots and pulmonary embolism, prompt medical intervention is essential. The main goal of treatment is to prevent the clot from growing larger and to reduce the risk of complications. Treatment options may vary depending on the severity of the clot and the individual’s overall health.
Anticoagulant medications, commonly known as blood thinners, are typically the first line of treatment for blood clots. These medications help prevent the formation of new clots and allow the body’s natural clot-dissolving mechanisms to work effectively. They can be taken orally or administered through injections, depending on the specific situation.
In some cases, thrombolytic therapy may be necessary. This involves the administration of medication to dissolve the clot more quickly. This approach is usually reserved for severe cases or when the clot is causing significant symptoms.
In rare instances, surgical intervention may be required. This can involve the removal of the clot or placement of a filter in the vein to prevent future clots from reaching the lungs.
Throughout the treatment process, close monitoring and follow-up with healthcare professionals are essential. This ensures that the treatment is effective and any potential side effects or complications are addressed promptly.
Remember, treatment for blood clots and pulmonary embolism should always be guided by healthcare professionals. If you or someone you know experiences symptoms or has been diagnosed with a blood clot or pulmonary embolism, seek medical attention immediately for proper evaluation and treatment. Don’t delay, as early intervention can make all the difference in preventing serious complications and saving lives.
Prevention of Blood Clots and Pulmonary Embolism
Prevention is always better than cure, especially when it comes to blood clots and pulmonary embolism. By taking proactive steps to prevent blood clots, you can significantly reduce your risk of developing these life-threatening conditions.
One of the most important preventive measures is staying active and avoiding prolonged periods of immobility. Whether you’re traveling or recovering from surgery, make sure to get up and move around frequently. Simple exercises like walking or stretching can help keep your blood flowing smoothly and prevent clots from forming.
Maintaining a healthy lifestyle is also crucial. Avoid smoking and limit your alcohol consumption, as these habits can increase your risk of blood clot formation. Eating a balanced diet and maintaining a healthy weight can also contribute to overall cardiovascular health and reduce your risk.
If you’re on hormonal contraceptives, talk to your healthcare provider about the potential risks and benefits. They can help you understand if you have any specific risk factors that may increase your chances of developing blood clots.
If you have any underlying medical conditions, make sure to manage them properly and follow your doctor’s recommendations. For example, if you have diabetes or heart disease, keeping your blood sugar and blood pressure under control can reduce your risk of clotting.
Lastly, if you’re planning long journeys or undergoing any surgeries, consult with your doctor about preventative measures, such as wearing compression stockings or taking blood thinners temporarily.
Remember, prevention is key when it comes to blood clots and pulmonary embolism. By taking control of your health, staying active, and following your doctor’s advice, you can reduce your risk and protect yourself from the silent killer. Stay informed, stay vigilant, and stay safe. Check out the American Blood Clot Association for more information.




